What causes Plantar Fasciitis?
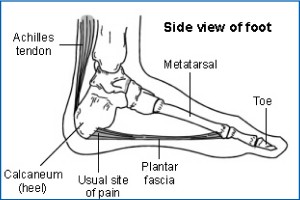
Plantar Fasciitis is inflammation of your Plantar Fascia. The Plantar Fascia is a strong band of tissue (like a ligament) that stretches from your heel to your middle foot bones. It supports the arch of your foot and also acts as a shock absorber.
Who is affected?
Plantar Fasciitis is a common foot condition. Approximately 1 in 10 people will have at least one episode of heel pain at some point in their life. It is common amongst runners and adults aged between 40 and 60 years old.

Diagnosis
Your GP, a Physiotherapist or a Podiatrist may be able to diagnose your pain by asking questions about your symptoms and examining your foot.
Symptoms
- Pain worse when taking your first step in the morning or after a long period of rest.
- Pain worse with sudden stretching movements e.g. going up stairs or standing on tip toes.
- Gentle exercises may help but long walks or being on your feet for long periods of time may aggravate pain.
- You may have a limp.
Prevention
- Regularly changing running shoes
- Wearing shoes with good cushion in heel and with arch support
- Lower your BMI if overweight
- Regular stretching
- Avoid exercise on hard surfaces
Physiotherapy
If your heel pain is affecting your activity and persisting, ask your GP about referral to a physiotherapist. Physiotherapy can help you to manage pain and improve your strength and flexibility. A physiotherapist can provide a variety of treatments, help you understand your problem and get you back to your normal activities. Physiotherapists can also give advice on how you can prevent symptoms returning in the future.
Treatment
Treatment for Plantar Fasciitis can include:
- Exercise
Exercise therapy will be one of the most important methods of treating this problem. See overleaf for for some exercises to get you started. The aim of these exercises is to increase your muscular flexibility.
- Strapping/Taping
At Blackstone your physiotherapist will be trained in the application of taping techniques designed to offload pressure on the heel and give your foot support.
- Footwear
Do not walk barefoot on hard surfaces. Choose shoes with cushioned heels and a good arch support, avoiding old or worn shoes that may not give a good cushion to your heel.
- Relative rest
Avoid walking long distances or prolonged standing.
- Ice
Pop a bottle of water in the freezer (500ml) and roll your foot over the top of this. Continue for ten minutes and repeat at least twice daily.
- Medication
Painkillers like paracetamol and ibuprofen may help and you should use them if you need to. Take them regularly and at the recommended dose to help you control pain and allow you to continue exercising. Consult your GP or pharmacist with regards which medicine you can and cannot take.

